Artificial intelligence is transforming every corner of the modern world, and nowhere is its impact more profound—or more complex—than in healthcare. From diagnosing diseases with superhuman accuracy to predicting patient outcomes and personalizing treatments, AI has the potential to revolutionize medicine. But alongside these breakthroughs come real challenges—ethical, technical, and regulatory.
As healthcare systems worldwide struggle with rising costs, physician burnout, and access disparities, AI is increasingly being looked to as a solution. However, the same technology that promises improved care also raises questions about privacy, accountability, and human oversight.
Here’s a closer look at how AI is reshaping healthcare today—and the concerns we must address to ensure it does more good than harm.
Major Innovations: Where AI Is Making an Impact
1. Diagnostics and Medical Imaging
AI’s strength in pattern recognition has made it especially powerful in diagnosing diseases from medical images. Deep learning algorithms can analyze X-rays, MRIs, and CT scans faster and sometimes more accurately than human radiologists.
Use cases:
- Breast cancer detection from mammograms
- Identifying lung diseases from chest X-rays
- Spotting retinal disorders in ophthalmology
Startups like Aidoc and Zebra Medical Vision and research efforts from institutions like Google Health have demonstrated how AI can reduce diagnostic errors, flag overlooked issues, and speed up triage.
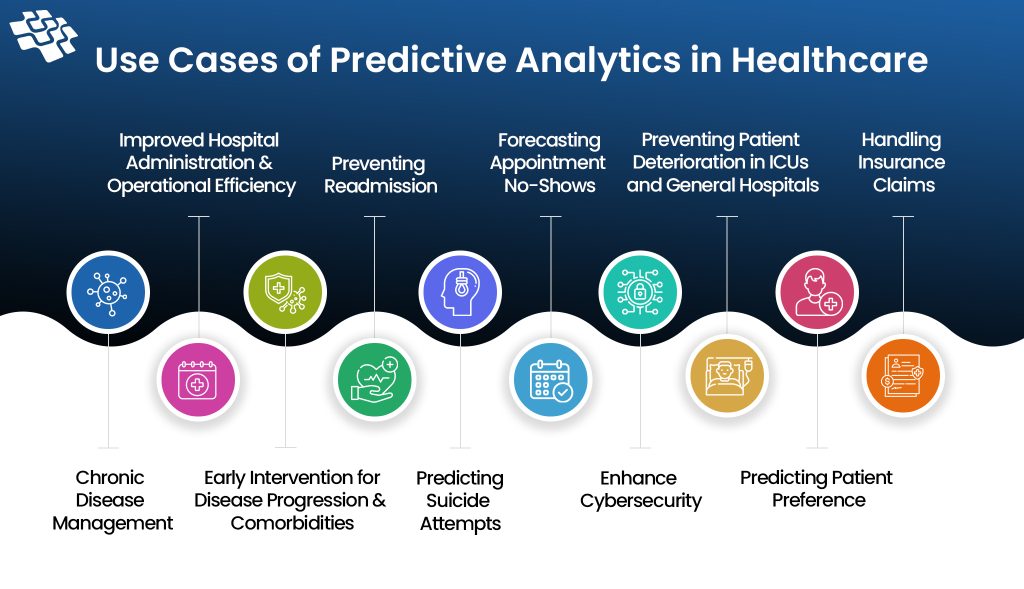
2. Predictive Analytics
AI can sift through electronic health records (EHRs), lab results, and wearable data to predict future health events. This proactive approach enables early intervention, which can reduce hospitalizations and improve outcomes.
Applications include:
- Predicting sepsis or heart failure risk in hospitalized patients
- Anticipating hospital readmission likelihood
- Detecting mental health deterioration based on behavioral and social indicators
3. Personalized Medicine
One-size-fits-all treatments are giving way to tailored care plans, thanks to AI’s ability to analyze genetics, lifestyle, and environmental data. By parsing through complex datasets, AI helps identify:
- Which cancer treatment might work best for a specific patient
- How a patient may respond to a certain medication
- Genetic mutations associated with rare diseases
AI-driven platforms are also speeding up drug discovery by modeling how molecules interact with proteins or predicting side effects before clinical trials.
4. Virtual Health Assistants and Chatbots
Conversational AI tools are being used to:
- Answer patient questions
- Schedule appointments
- Provide medication reminders
- Triage symptoms
These systems reduce administrative burdens on healthcare providers and offer round-the-clock support to patients, especially in primary care and mental health contexts.
5. Robotics and Surgery
While AI is not replacing surgeons, it is enhancing surgical precision. Robotic systems guided by AI can assist in minimally invasive procedures, improving outcomes and reducing recovery times. Machine learning can also help monitor vital signs in real time during surgery to flag potential issues.
Benefits: Why the AI Surge in Healthcare Matters
- Faster, More Accurate Diagnoses: AI reduces diagnostic time and can outperform humans in certain domains.
- Operational Efficiency: Hospitals can automate scheduling, billing, and supply chain management using AI.
- Improved Access to Care: AI chatbots and remote monitoring tools extend healthcare to underserved regions.
- Enhanced Clinical Decision-Making: Physicians gain data-backed insights to make more informed choices.
- Cost Reduction: Early detection and preventive care can lower long-term treatment costs.
Major Concerns and Challenges
While AI’s promise in healthcare is vast, it comes with real risks—some technical, others human.
1. Bias and Inequity
AI systems learn from data, and if that data reflects societal or institutional biases, the model can perpetuate them. For example:
- A skin cancer detection tool may underperform on darker skin tones if trained mostly on lighter ones.
- Predictive tools might offer less accurate results for underrepresented populations, such as minorities or women.
Without diverse and representative data, AI can unintentionally worsen health disparities.
2. Data Privacy and Consent
Healthcare data is among the most sensitive information a person owns. AI systems often require access to vast amounts of personal medical data, raising questions like:
- Who owns the data?
- How is consent obtained and managed?
- What happens if the data is breached or misused?
Regulations like HIPAA in the U.S. and GDPR in Europe aim to safeguard privacy, but enforcement in the age of AI is complex and evolving.
3. Lack of Transparency (“Black Box” Problem)
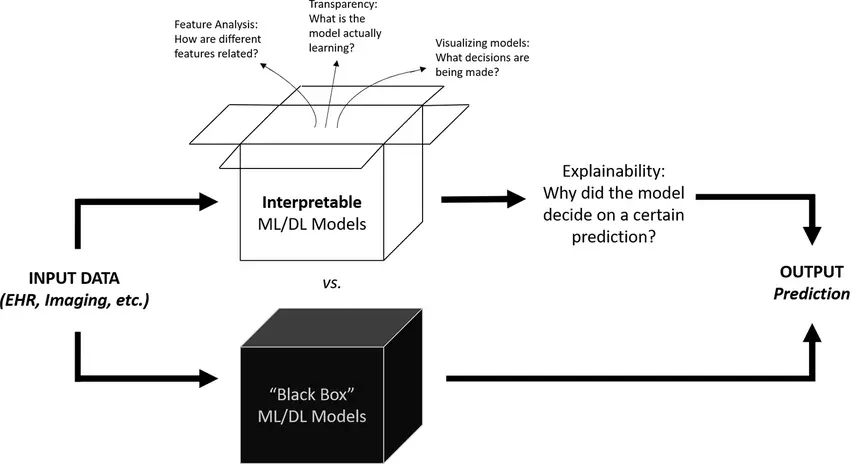
Many AI models—especially deep learning systems—are difficult to interpret. Even their developers may not fully understand how the algorithm arrived at a particular decision. This lack of transparency poses a problem in healthcare, where explainability is crucial for:
- Clinical accountability
- Gaining physician trust
- Justifying treatment decisions to patients
4. Regulatory Hurdles
Most countries’ healthcare regulations were not designed with AI in mind. The FDA and other regulators are developing new frameworks for “Software as a Medical Device” (SaMD), but questions remain:
- How often should AI tools be re-evaluated?
- How do we assess algorithm updates that change model behavior?
- Who is liable if an AI makes a mistake?
Balancing innovation with patient safety is a delicate process.
5. Job Displacement and Workflow Integration
AI may not replace doctors, but it could change the nature of healthcare jobs significantly. Radiologists, for instance, may spend more time interpreting AI results than examining raw scans.
Introducing AI into clinical settings also requires:
- Training staff to work with new tools
- Redesigning workflows to integrate AI effectively
- Ensuring the tech adds value without disrupting care
The Role of Human-AI Collaboration
Rather than viewing AI as a replacement for human providers, the most successful use cases involve collaboration. The vision is for AI to handle repetitive, data-heavy tasks—freeing clinicians to focus on empathy, decision-making, and personalized care.
For instance:
- An AI may detect signs of pneumonia in a chest X-ray, but a physician considers the patient’s full history before prescribing treatment.
- A chatbot may monitor a patient’s mental health trends, but a therapist provides context and intervention.
Human oversight remains critical for safety, trust, and ethical alignment.
The Path Forward: Building Responsible AI in Healthcare
To realize AI’s full potential in healthcare, we need to focus on responsible innovation. This means:
- Prioritizing fairness and inclusion in training data
- Enforcing transparency and explainability standards
- Creating robust regulatory frameworks for safety and accountability
- Engaging patients and clinicians in the design and deployment of AI tools
- Ensuring accessibility and affordability of AI-driven care
AI is not a silver bullet, but with thoughtful design and oversight, it can be one of the most powerful tools in the fight for a healthier future.
Conclusion
AI is no longer a futuristic idea in healthcare—it’s already here, assisting in diagnoses, guiding treatments, and streamlining hospital operations. Its innovations promise better outcomes, improved access, and more efficient systems.
But these gains come with risks we can’t ignore. Bias, transparency, privacy, and accountability must be addressed head-on. As the industry moves forward, the guiding principle must be clear: technology should serve humanity, not replace it.
The future of healthcare is being shaped now—and it’s up to all of us to make sure that future is safe, ethical, and equitable.